nalco group
bone, muscle & joint pain physio
BOOK NOW / WHATSAPP ABOUT YOUR PAIN OR INJURY
- ORCHARD 400 Orchard Road #12-12 Singapore 238875
- TAMPINES 9 Tampines Grande #01-20 Singapore 528735
- SERANGOON 265 Serangoon Central Drive #04-269 Singapore 550265
Home > Blog > Physiotherapy > Conditions > Jaw Fracture (Temporomandibular Joint Fracture) Physiotherapy
Jaw Fracture (Temporomandibular Joint Fracture) Physiotherapy
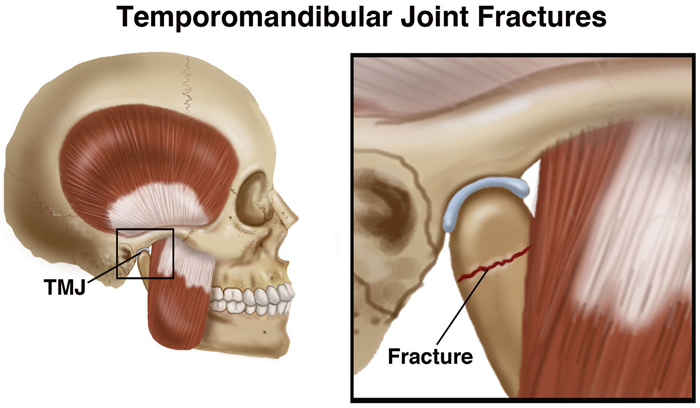
Temporomandibular Joint (TMJ) fracture (jaw fracture) is the second most common fracture to the bones of the face - second only when compared to the bones of the nose which are broken more frequently.
The jaw bone (termed as mandible) or skull bone section of the jaw (temporal bone) can also be broken near or through the TMJ. The injury normally occurs due to trauma to the face, such as a direct hit.
The joint itself can be damaged as well as the muscles that move the jaw ie patients can injure/fracture the bone, the joint of the temporomandibular joint and the muscles of the TMJ too.
After the bone heals, it may be difficult to open or move
the jaw. Physical therapists help people who have sustained TMJ
fractures to relieve their pain and restore movement and function to the
jaw.
What Is Temporomandibular Joint Fracture (Jaw Fracture)?
A temporomandibular joint (TMJ) facture happens when the mandible and/or temporal bone is suffers a breakage or fracture near or through the TMJ, which is the joint connecting the jaw bone to the skull.
Like other bones in the body, our mandible, also known as our jaw bone, and the temporal bone, which is the bone on the skull that forms the upper part of the jaw joint, can break when subjected to trauma.
TMJ fractures typically happen due to direct trauma to the face - the jaw most often breaks along the condyles, which are rounded projections on the jaw bone. Fractures also may occur with a dislocation of the temporomandibular joints.
The most common causes of TMJ fracture includes:
- motor vehicle accidents
- falls
- assault
- sports injuries
Men aged 20 to 29 years are most likely to sustain these injuries, and are approximately 3 times more likely than women of the same age to do so.
Following a TMJ fracture, especially if the inside surface of the mouth is torn, there also is a risk of infection, which can lead to osteomyelitis of the jaw. If patient suffer damage or blows to the head severe enough to cause a TMJ fracture, it can also cause a concussion.
How Does it Feel?
Following a TMJ fracture, you may experience:
- Jaw pain
- Swelling and possible bruising in the area
- Jaw fatigue
- Difficulty opening your mouth to eat or talk
- Ringing in your ears
- Dizziness
- Headache
- Loose or broken teeth
- Popping sounds in your jaw
- Neck pain
- A change in the way the teeth fit together
- A locking jaw
- A bump you can feel with your fingers on the jaw bone or joint
How Is temporomandibular joint (TMJ) fracture Diagnosed?
In cases of facial trauma and pain, diagnosis is made by an emergency medicine doctor at a hospital or other emergency clinic. X-rays or computed tomography (CT scan) will be ordered to determine the existence and severity of a fracture.
If the jaw was/has been dislocated, the physician will return it to its normal position.
- A less severe fracture is diagnosed when the bone is still in place, but has a small fracture line where the bone has broken.
- A more severe fracture can involve a larger fracture line, partially displaced sections of bone, or a dislocation.
- An extreme fracture involves displaced segments of bone or fragmented bone, with a significant alteration of bone structure.
There are several treatments to help a TMJ fracture safely heal.
- If the fracture is less severe, your physician will recommend resting the jaw by:
- Eating soft foods, or going on a liquid diet.
- Limiting jaw use such as speaking or brushing your teeth.
- If the fracture is severe, your physician may consider a form of splint therapy to hold the jaw steady and rest it in a proper position for healing.
- If the fracture is extreme, surgery may be required, or the jaw may be set and wired closed to prevent any movement and ensure complete healing.
All of these treatments allow the jaw to heal, but often result in TMJ stiffness.
The muscles used to move the jaw also may become tight and weak. You may not be able to eat, drink, or open your mouth as you normally would. Our senior physiotherapist will work with you to help restore your jaw's normal movement, function, and muscular strength.
how our senior physiotherapists can help
Once you have completed a course of rest and/or splinting, we can help restore the natural movement of your jaw and decrease your pain.
During your first visit, our senior physical therapist may:
- Review your medical history, and discuss any previous surgery, fractures, or other injuries to your head, neck, or jaw
- Evaluate the quality and quantity of movement of your jaw and neck
- Assess your posture and observe how your neck moves
- Examine the TMJ to find out how well it can open, and whether there are any abnormalities in jaw motion following the fracture
Following the examination, we will select the appropriate treatments to improve your jaw movement and relieve your pain.
Improving Your Jaw Movement
Stretching and Motion Exercises
We may prescribe stretches and range-of-motion exercises for the jaw. The instruction will include guidelines for frequency and intensity of movement to ensure your safe performance of all your exercises.
Manual Therapy
We may also apply skilled hands-on techniques (manual therapy) to gently increase your jaw movement and relieve your pain.
"Low-Load" Exercises
We may teach you special "low-load" strengthening exercises that don't exert a lot of pressure on your TMJ, but can help strengthen the muscles of the jaw and restore a more natural, pain-free motion. We also will teach you exercises that help you increase the opening of your jaw and improve the way it works.
Relieving Your Pain
If your pain is severe, we may apply physical modalities, such as electrical stimulation or deep heat, to reduce pain and improve motion.
